【2026 Guide to Gum Disease】Cost, Symptoms, and Causes Explained
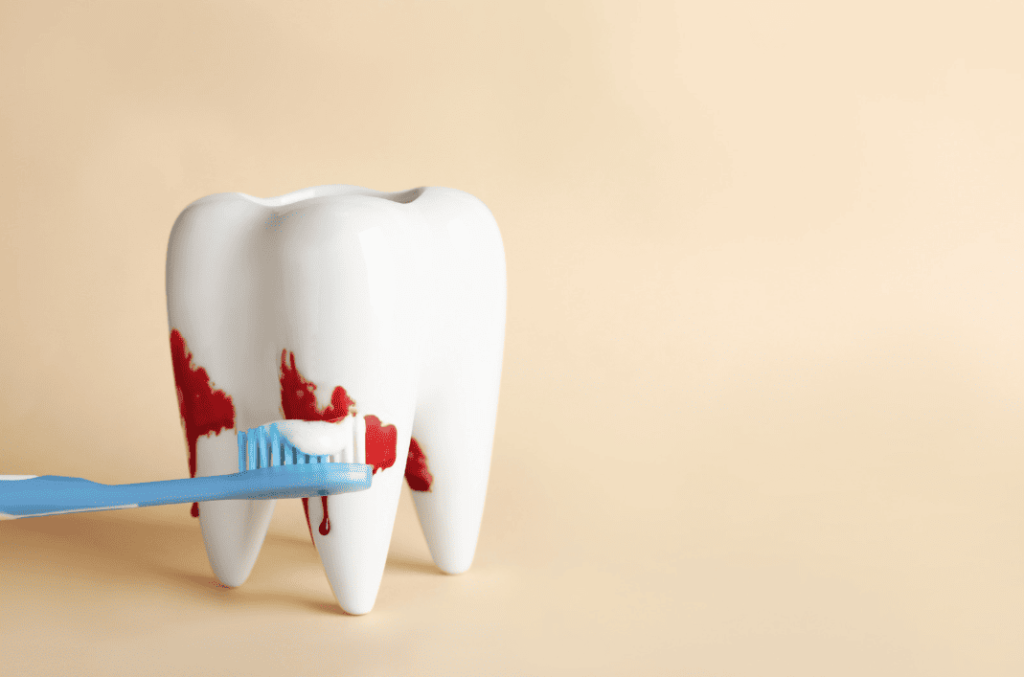
Periodontal Disease (Gum Disease) is often called the “silent killer” of teeth. Many people mistake bleeding gums for “heatiness” or brushing too hard, unaware that these are early warning signs of infection. If left untreated, gum disease can lead to receding gums, loose teeth, and eventually, total tooth loss.
This article provides the 2026 updated treatment costs, a 30-second self-test, and an in-depth look at the differences between “Deep Cleaning” and “Regular Cleaning” to help you protect your oral health during the golden treatment window.
Quick Summary: 4 Key Points of Gum Disease Treatment
- ⚠️ Warning Signs: Periodontal disease is often painless. Bleeding gums, persistent bad breath, and widening gaps between teeth mean the “foundation” supporting your teeth is beginning to collapse.
- 🦷 Treatment: Regular cleaning cannot cure deep-seated inflammation. “Deep Cleaning” (Root Planing) reaches more than 5mm below the gum line to remove bacterial strongholds and is the last line of defense for saving your natural teeth.
- 💰 2026 Estimated Costs: Deep cleaning costs approximately $3,000 – $8,000 per quadrant; periodontal surgery starts from approximately $5,200. (Click to view full fee schedule)
- 🔴 Reality Check: Periodontal disease is irreversible. Lost alveolar bone cannot naturally regenerate. The earlier the treatment, the higher the success rate and the lower the cost.
30-Second Self-Test: Do You Have Warning Signs?
In its early stages, gum disease is often painless and easy to ignore. Take 30 seconds to check if you have any of the following symptoms:
- [ ] Gums bleed during brushing or flossing (The most common early warning sign)
- [ ] Red, swollen, or tender gums (Healthy gums should be firm and pale pink)
- [ ] Persistent bad breath or a bad taste in the mouth that won’t go away
- [ ] Receding gums, making your teeth look longer or causing sensitivity
- [ ] Developing gaps between teeth where food frequently gets stuck
- [ ] Loose or shifting teeth, or a change in how your teeth fit together when you bite
- [ ] Pus appearing between your teeth and gums (Periodontal abscess)
Your Results:
- 1-2 Items: You may have early-stage Gingivitis. We recommend booking a professional cleaning and check-up as soon as possible to reverse the condition.
- 3 or More Items: You may have progressed to Periodontitis (moderate to severe gum disease). It is critical that you seek professional dental assistance immediately to prevent tooth loss.

The Mechanism of Disease: Why Do Teeth Fall Out “Silently”?
It is a major misconception that “no cavities = healthy teeth”. While cavities destroy the tooth itself, periodontal disease destroys the foundation system supporting the tooth.
Think of your teeth as a building: the gums are the lawn, and the alveolar bone is the deep concrete foundation. If the foundation is lost, even a perfectly intact building (tooth) will become unstable and collapse.
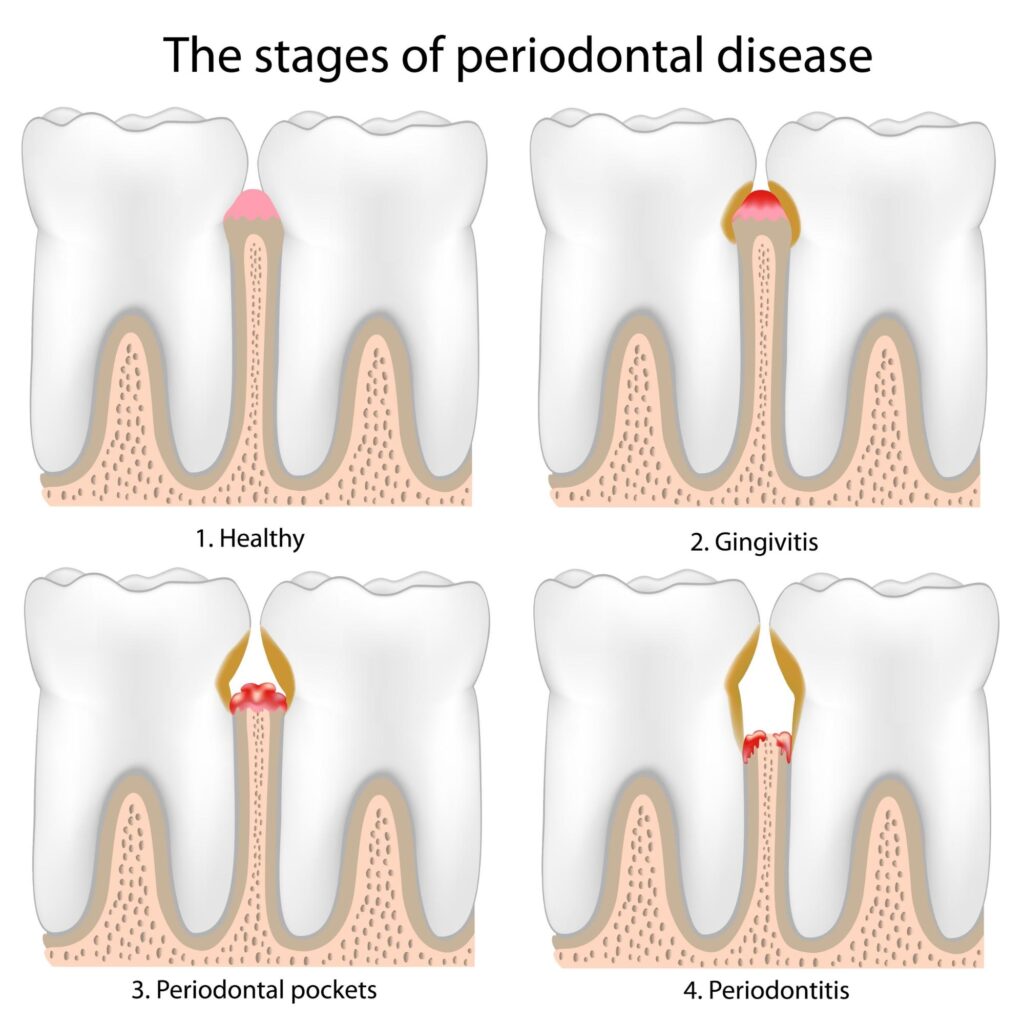
The 4 Stages of Foundation Collapse:
1. Bacterial Biofilm: The Invisible Invaders
Within minutes after eating, bacteria form a sticky film on the tooth surface. This is a highly organized “biofilm” that regular mouthwash cannot penetrate. If not physically removed by correct brushing within 24 hours, it begins to transform.
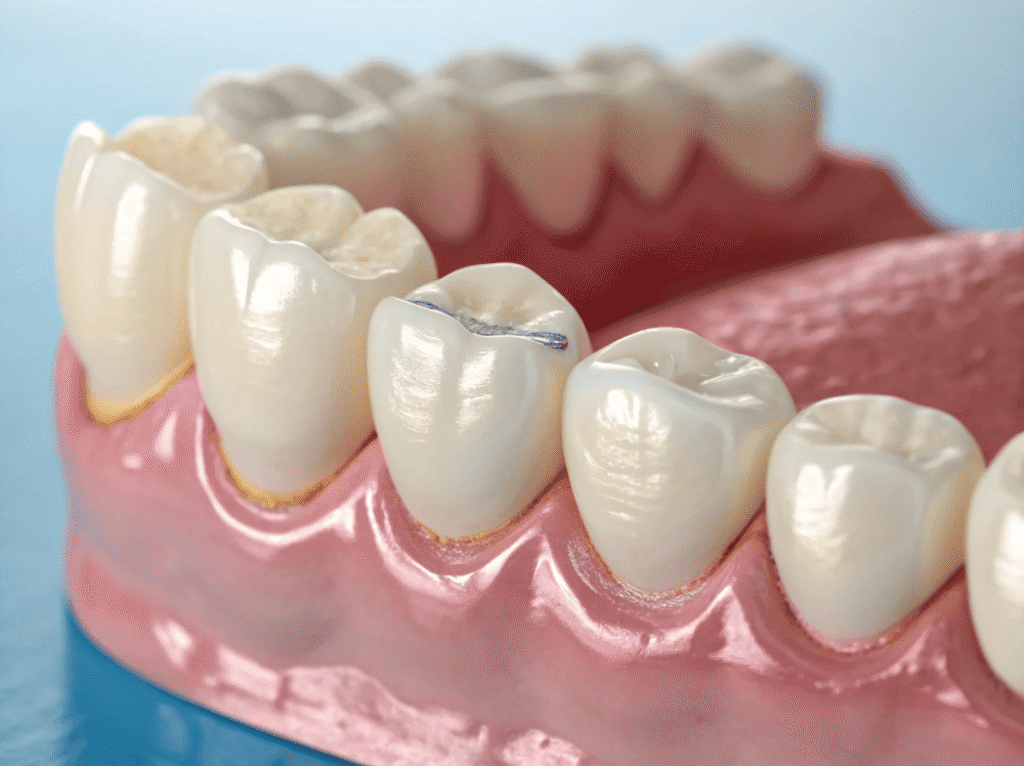
2. Calculus Fortress: Bacterial Reinforced Concrete
Unremoved biofilm absorbs minerals from saliva and hardens into “calculus” (tartar). Calculus is rough and toxic, attracting more bacteria and creating a “bacterial base” that cannot be brushed away, constantly irritating the gums.
3. Periodontal Pocket Formation: An Oxygen-Free Breeding Ground
Chronic inflammation causes the gum tissue to pull away from the tooth, creating a gap known as a “Periodontal Pocket”. When the pocket depth exceeds 4mm, it becomes an oxygen-free environment—ideal for highly toxic “anaerobic bacteria” to multiply rapidly.
4. Bone Erosion: The Ultimate Collapse
To fight deep-seated bacteria, the body’s immune system triggers an inflammatory response. While attacking bacteria, immune cells accidentally damage the periodontal ligaments and alveolar bone, leading to bone resorption and foundation shrinkage. Once the supporting bone is reduced by more than 50%, the tooth becomes loose and eventually falls out, even if there are zero cavities.
*Professional Note: Because there are no pain nerves inside the alveolar bone, this process is usually painless. Patients often do not seek help until they feel weak when chewing or notice loose teeth, by which time treatment complexity and costs have significantly increased. This is why we emphasize the importance of professional periodontal assessments and cleanings every 6 months.

Bleeding Gums or Gum Pain? Get Expert Treatment Today!
If you’re experiencing persistent gum issues such as:
- ✅ Bleeding or swollen gums when brushing or flossing
- ✅ Persistent bad breath or a bad taste in your mouth
- ✅ Receding gums exposing tooth roots
- ✅ Loose teeth or discomfort while chewing
Our Dental Clinics Offer Comprehensive Gum Disease Treatment, Including:
- 🦷 Deep Cleaning: For early-stage gum disease, we offer thorough cleaning to remove plaque and tartar.
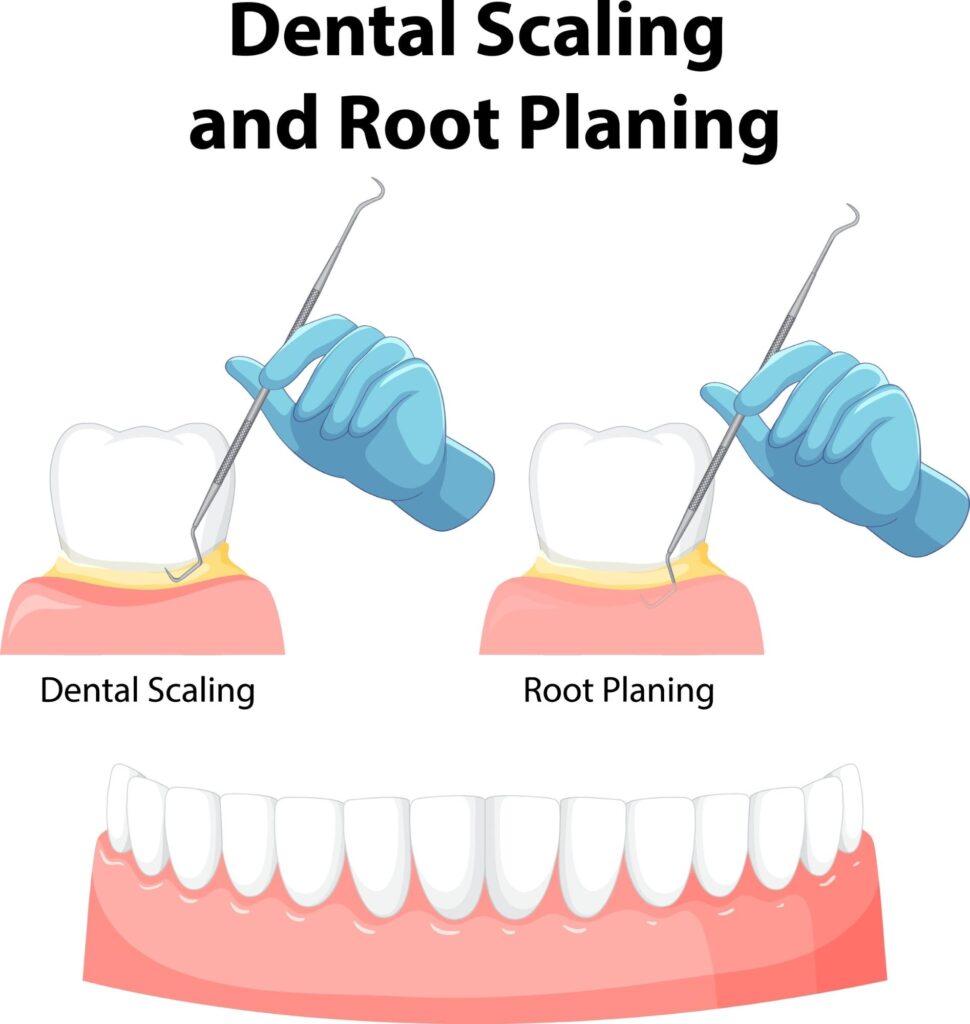
- 🦷 Scaling and Root Planning: This deep-cleaning procedure removes bacteria from below the gum line and smooths the tooth root to promote healing.
- 🦷 Antibiotic Therapy: We may prescribe antibiotics to control bacterial infection.
- 🦷 Surgical Procedures: For advanced cases, we offer surgical options like flap surgery and bone and tissue grafts, full mouth restorations. We have Periodontal specialists in our team for treating advanced gum disease cases.
Smith & Jain Dentists in Central Hong Kong | Same-Day Appointments Available
2026 Gum Disease Treatment Fee Reference
Fees may vary based on the severity of the condition (e.g., number of teeth requiring treatment, need for surgery, or specialist involvement). The following fees are referenced from The Prince Philip Dental Hospital (PPDH) private patient fee schedule as a budget indicator:
Treatment Item | Price Range (HKD) | Remarks |
Non-surgical Periodontal Therapy (per quadrant) | $3,000 – $8,000 | Also known as “Deep Cleaning” or “Root Planing.” The mouth is typically divided into 4 quadrants. |
Periodontal Surgery (per quadrant) | $5,200 – $10,000 | Advanced treatment for deep periodontal pockets (e.g., Flap Surgery). |
Periodontal Regenerative Surgery | $5,000 – $15,000 | Aims to regrow bone. Bone graft material or regenerative membranes are charged separately. |
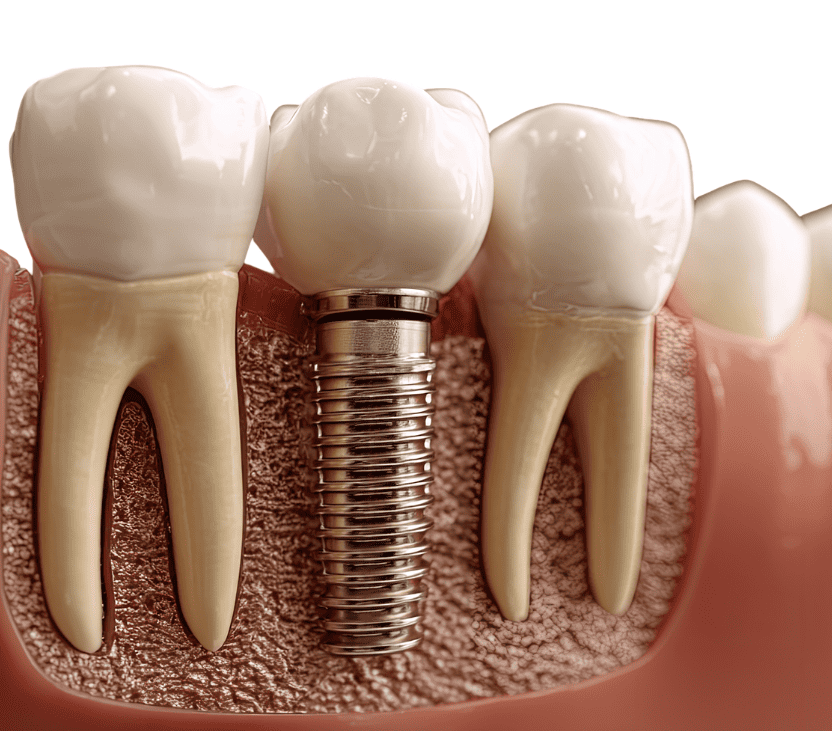
Managing Peri-implant Biological Complications | $3,000 – $10,000 | Specialized care for inflammation around existing dental implants (Peri-implantitis). |
Periodontal Splinting (per tooth) | $1,000 – $2,000 | Used to stabilize loose teeth and improve chewing stability. |
Supportive Periodontal Care | $500 – $1,500 | Regular follow-ups, maintenance, and specialized cleaning after treatment completion. |
Note: The above prices are for reference only. Actual fees depend on the clinic’s equipment, the doctor’s experience, and the complexity of the case. We recommend consulting your dentist for an accurate quote before starting treatment.

“Regular Cleaning” vs. “Deep Cleaning”: Which Should I Choose?
Many patients ask, “I have my teeth cleaned every year, why do I still have gum disease?” The key lies in the “cleaning depth.” Regular cleaning only handles visible calculus, while the threats of periodontal disease are often hidden in “invisible” depths.
Regular Cleaning: Daily “Surface Maintenance”
Regular scaling is the foundation of dental care, primarily targeting areas above the gum line.
- Ideal for: Patients with healthy oral conditions, mild gingivitis, or those attending half-yearly preventive check-ups.
- Scope: Removes surface stains (tobacco, tea), soft debris, and calculus accumulated at the gum margin.
- Experience: Usually requires no anesthesia; involves slight vibrations or water spray.
- Purpose: Prevents inflammation and maintains gum health.
Deep Cleaning: “Deep Debridement” of the Foundation
When periodontal pockets exceed 4mm, bacteria have already invaded below the gums, reaching areas regular instruments cannot touch.
- Ideal for: Patients diagnosed with moderate to severe periodontal disease, deep pockets, or signs of bone loss.
- Scope: Reaches deep into the periodontal pockets to scrape away bacterial strongholds and deep-seated calculus attached to the root surfaces.
- Experience: To ensure comfort while cleaning deep gum tissues, this is typically performed under local anesthesia.
- Purpose: To smooth infected root surfaces, eliminate bacterial toxins, and allow inflamed gums to firmly “re-grip” the roots, preventing further foundation loss.
Comparison at a Glance
Feature | Regular Cleaning (Scaling) | Deep Cleaning (Root Planing) |
Cleaning Depth | Above the gum margin | Deep below the gums (Pockets) |
Goal | Prevent gum inflammation | Control disease; Save natural teeth |
Anesthesia | Usually not required | Usually required (Local) |
Time Required | Approx. 30–45 minutes | Per quadrant; approx. 1 hour per session |
Professional Advice:
If you experience abnormal pain during a cleaning or if your dentist discovers deep periodontal pockets, regular cleaning is no longer enough to protect your teeth. While deep cleaning has a higher initial cost, it is your final line of defense to avoid spending tens of thousands on future implants or dentures.

Periodontal Treatment Journey
Periodontal treatment is not a one-time fix but a systematic, step-by-step process. The core objectives are to eliminate the source of infection, reduce periodontal pockets, stabilize the tooth structure, and transition into long-term maintenance.
Phase 1: Clinical Diagnosis and Risk Assessment
Before starting any treatment, the dentist must gather precise data on the damage to the periodontal tissues:
- Full-Mouth Periodontal Probing: A periodontal probe is used to measure the Pocket Depth around each tooth. Depths exceeding 4mm typically indicate inflammation, while depths over 6mm signify severe disease.
- Radiographic Evaluation: Using full-mouth X-rays (OPG) or Cone Beam Computed Tomography (CBCT) to assess vertical and horizontal bone loss and determine the prognosis of the teeth.
- Risk Factor Analysis: Evaluating the patient for habits like smoking, or systemic diseases like diabetes that affect the immune system.
Phase 2: Non-Surgical Basic Therapy
This is the cornerstone of all periodontal therapy, controlling over 80% of early to moderate cases:
- Deep Cleaning and Scaling & Root Planing (SRP): Performed under local anesthesia, specialized instruments are used to reach below the gum line to thoroughly remove calculus, bacterial biofilm, and infected tissue. This smoothes the root surface, allowing the gums to reattach properly.
- Biofilm Control Education: Professional guidance on using targeted home care tools, such as interdental brushes or single-tuft brushes, which is essential for long-term success.
Phase 3: Re-evaluation of Treatment Response
The 6 to 8 weeks following treatment is the critical window for tissue healing:
- Healing Indicator Check: Re-measuring pocket depths and the Bleeding on Probing (BOP) index. If pockets have shrunk and bleeding has stopped, the patient enters the maintenance phase.
- Determining Next Steps: If pockets deeper than 5-6mm persist with ongoing inflammation, surgical intervention may be considered.
Phase 4: Periodontal Surgical Therapy (As Needed)
When basic therapy cannot completely clear bacteria from deep, unreachable areas, surgery is required:
- Periodontal Flap Surgery: A minimally invasive procedure where the gums are folded back to provide a direct view for thorough root debridement and reshaping of irregular bone contours.
- Periodontal Regeneration: For specific bone defects, artificial bone grafts or Guided Tissue Regeneration (GTR) membranes can be placed to stimulate the regrowth of lost periodontal tissue and strengthen the foundation.
Phase 5: Supportive Periodontal Therapy and Maintenance
Periodontal disease is a chronic condition that can easily recur if bacteria accumulate again:
- High-Frequency Follow-ups: Recovered patients are advised to have professional check-ups and cleanings every 3 to 4 months, rather than the traditional six-month interval.
- Long-term Monitoring: Regular monitoring of gum recession and bite changes ensures stable results and extends the lifespan of natural teeth.
How Can You Prevent Periodontal Disease?
Periodontal disease is a condition that can be managed but is difficult to fully cure once damage has occurred. Therefore, prevention is always more critical than treatment. Through consistent home care and regular professional check-ups, you can significantly reduce the risk of the disease occurring or recurring.
Here are the effective prevention methods recommended by dentists 👇
🏠 Home Prevention Habits: Maintaining Healthy Gums Every Day
✅ 1. Correct Brushing Technique (The Bass Method) Brush your teeth at least twice a day (morning and night) for 2–3 minutes each time. The key is “technique” rather than “force.” The Bass Method allows bristles to reach deep into the gum line, effectively removing plaque and preventing gingivitis and periodontal disease.
Recommended Practice:
- Place the toothbrush at a 45° angle to the gums and use a gentle, vibrating back-and-forth motion.
- Use a soft-bristled toothbrush or an electric toothbrush to avoid damaging the gum tissue.
- Replace your toothbrush every 3 months.
✅ 2. Daily Flossing or Interdental Brushing Brushing alone cannot clean the tight spaces between teeth. Using dental floss or interdental brushes daily effectively removes plaque and food debris hidden between teeth, reducing the chance of gum inflammation.
Interdental Brush Guide: How to Choose and Use It?
✅ 3. Diet and Lifestyle Management
- Reduce sugary and sticky foods: Sugar promotes bacterial growth and accelerates plaque formation.
- Quit smoking and limit alcohol: Excessive smoking and alcohol consumption are high-risk factors for periodontal disease, as they reduce blood flow to the gums and impair the body’s healing capabilities.
- Balanced diet: Consume foods rich in Vitamin C (such as kiwis, oranges, and bell peppers) to aid in gum repair and tissue health.
✅ 4. Manage Stress Levels Chronic stress or teeth grinding (bruxism) can indirectly lead to gum recession and periodontal issues. Maintaining good sleep hygiene and moderate exercise helps boost your overall immune system.
🏥 Professional Dental Prevention: Regular Check-ups are Key
✅ 1. Regular Scaling and Dental Exams Even with diligent daily brushing, it is difficult to remove tartar (calculus) hidden below the gum line. We recommend a professional scaling every 6 months to remove tartar from above and below the gums to keep the periodontium clean.
- Note: For high-risk patients (e.g., smokers, diabetics, or those with a history of gum disease), this interval should be shortened to every 3–4 months.
✅ 2. Regular Periodontal Health Assessment Your dentist will track changes in your periodontal health by:
- Measuring Periodontal Pocket Depth (PPD)
- Evaluating the Bleeding on Probing (BOP) index
- Observing gum recession and the condition of the alveolar bone
- This allows for the early detection of potential problems.
✅ 3. Ongoing Oral Hygiene Education Through guidance from your dentist or dental hygienist, learning the brushing techniques and cleaning tools best suited to your specific oral condition is effective for maintaining long-term gum stability.
Bleeding Gums or Gum Pain? Get Expert Treatment Today!
If you’re experiencing persistent gum issues such as:
- ✅ Bleeding or swollen gums when brushing or flossing
- ✅ Persistent bad breath or a bad taste in your mouth
- ✅ Receding gums exposing tooth roots
- ✅ Loose teeth or discomfort while chewing
Our Dental Clinics Offer Comprehensive Gum Disease Treatment, Including:
- 🦷 Deep Cleaning: For early-stage gum disease, we offer thorough cleaning to remove plaque and tartar.
- 🦷 Scaling and Root Planning: This deep-cleaning procedure removes bacteria from below the gum line and smooths the tooth root to promote healing.
- 🦷 Antibiotic Therapy: We may prescribe antibiotics to control bacterial infection.
- 🦷 Surgical Procedures: For advanced cases, we offer surgical options like flap surgery and bone and tissue grafts, full mouth restorations. We have Periodontal specialists in our team for treating advanced gum disease cases.
Smith & Jain Dentists in Central Hong Kong | Same-Day Appointments Available
Frequently Asked Questions About Gum Disease
What is gum disease, and how serious is it?
Gum disease (periodontal disease) is a bacterial infection that affects the gums and bones supporting the teeth. It starts with mild gum inflammation (gingivitis) and can progress to severe periodontitis, which can lead to tooth loss if untreated.
How do I know if I have gum disease?
Common signs of gum disease include:
- Bleeding gums, especially when brushing or flossing
- Red, swollen, or tender gums
- Bad breath or a persistent bad taste in the mouth
- Gum recession (teeth appearing longer)
- Loose teeth or widening gaps between teeth
- Pus between teeth and gums
If you notice any of these symptoms, see a dentist as soon as possible.
What causes gum disease?
The primary cause is plaque buildup due to poor oral hygiene. Other risk factors include:
- Smoking and tobacco use
- Uncontrolled diabetes
- Hormonal changes (pregnancy, menopause)
- Poor diet and nutritional deficiencies
- Stress, which weakens the immune system
- Genetic predisposition
Can gum disease be reversed?
The early stage (gingivitis) can be reversed with good oral hygiene and professional cleanings. However, advanced gum disease (periodontitis) cannot be fully reversed but can be managed with proper treatment.
How is gum disease treated?
Non-Surgical Treatments:
- Deep cleaning (Scaling & Root Planing, SRP): Removes plaque and tartar under the gums
- Antibiotics: Used in rinses or gels to control infection
- Laser therapy: Targets infected tissue with minimal discomfort
Surgical Treatments (for severe cases):
- Flap surgery: Removes deep plaque deposits and reshapes bone
- Gum grafting: Restores receded gums
- Bone grafting: Rebuilds bone lost due to infection
Is gum disease painful?
Early gum disease (gingivitis) is usually painless. As it progresses, you may feel gum tenderness, discomfort while eating, or tooth sensitivity. Advanced gum disease can cause pain due to infection and tooth movement.
How often should I see a dentist if I have gum disease?
Patients with gum disease should have professional cleanings every 3 to 4 months instead of the usual 6-month checkups. Your dentist will advise on a suitable schedule based on your condition.
Can gum disease lead to other health problems?
Yes. Research links gum disease to:
- Heart disease and stroke
- Diabetes complications
- Pregnancy risks (preterm birth, low birth weight)
- Respiratory infections
Treating gum disease can help reduce the risk of these health problems.
Does gum disease cause bad breath?
Yes. Bacteria trapped under the gums release toxins that cause persistent bad breath (halitosis). Proper treatment and oral hygiene can help eliminate it.
Can children get gum disease?
Yes, but it is less common. Poor oral hygiene, genetic factors, and medical conditions can contribute to gum disease in children and teenagers.
What happens if gum disease is left untreated?
Untreated gum disease can lead to:
- Chronic bad breath
- Receding gums
- Loose or shifting teeth
- Tooth loss
- Jawbone deterioration
Can gum disease affect my ability to eat?
Yes. Severe gum disease can cause pain when chewing, loose teeth, and sensitivity, making it difficult to eat certain foods. Treating gum disease early helps prevent these issues.
Can gum disease come back after treatment?
Yes, if oral hygiene is not maintained. Regular dental visits, proper brushing, and flossing can help prevent recurrence.
Disclaimer
All information provided on this website is for informational purposes only and is intended to help readers gain general knowledge about dental health. The content on this website should not be considered a substitute for professional dental diagnosis, advice, or treatment. If you have any dental concerns, please consult a licensed dentist for appropriate medical advice and treatment.
While we strive to ensure the accuracy and completeness of the information provided, we do not guarantee that all content is always up-to-date or applicable to individual circumstances. Smith & Jain Dentists and its affiliates are not responsible for any direct or indirect damages resulting from the use of this website’s information.
This website may include links to external websites for reference purposes only. Smith & Jain Dentists is not responsible for the content or accuracy of third-party websites.